How Long Does Spinal Surgery Take

The spinal surgery David B. underwent in November wasn't his first – just information technology was the commencement time he was awake for a procedure.
David is i of about 10 patients so far who have taken reward of UC San Francisco's offering of awake spine surgery, which neurosurgeon Praveen Mummaneni, MD, began doing in spring of 2018.
"At first I thought 'Do I really want to be awake for this?'" said David. But in reality, it was more like being pleasantly oblivious. "I was not aware of annihilation that was going on. It was sleepy time."
Later the process – a transforaminal lumbar interbody fusion, or TLIF, which generally takes only two to 3 hours – David was up and walking over again, without pain, before the end of the twenty-four hours.
"The procedure is relatively new," said Mummaneni, who is also co-director of the UCSF Spine Center. "Information technology's changing my do in that I tin get my patients through their surgery much more quickly."
Local Anesthetic Lends Advantages Over Going to Slumber
1 of the keys to this new approach to spine surgery is a long-acting, local coldhearted called liposomal bupivacaine, which was recently approved by the U.Southward. Food and Drug Administration. The anesthetic is injected into muscle in the low back before the incision is made, and provides hurting relief for 72 hours.
"This means we're not giving postal service-operative IV narcotics anymore," said Mummaneni. "And it's allowed us to cutting the hospital stay by two-thirds."
A traditional spinal fusion surgery with general anesthesia takes virtually four hours and requires a hospital stay of three to four days every bit well every bit Iv painkillers. The awake spine surgery takes half the time and typically has patients out of the hospital within 24 hours.
Patients might keep oral pain medication for a week or two afterward the long-acting anesthetic wears off, but overall the pain direction is much less intensive.
The benefits of awake spine surgery go beyond quick recovery times and shorter hospital stays. Patients circumvent the disorientation and "out-of-it" country that anesthesia and post-operative narcotics induce, and return to their lives in much shorter order. And the lack of general anesthesia means that patients don't need to exist on a ventilator or breathing tube during surgery, reducing the risk of side effects such as post-operative nausea and delirium.
Low Back Pain Takes Concrete, Economic Toll
In that location's no shortage of people in the U.Due south. in need of back surgery. Spinal disorders debilitate more than Americans than whatever other medical status. Nearly four in five Americans struggle with low dorsum hurting at some point in life. About one-quarter of those, or xx percent of Americans, experience chronic low back pain with persistent symptoms, according to the National Institutes of Health.

Well-nigh iv in five Americans struggle with low back pain at some point in life.
The incidence of depression back pain has been steadily increasing since the 1990s, is now the leading cause of missed workdays and the most common cause of job-related disability, according to the National Institutes of Health.
Because back pain interferes with an individual's ability to practise and be agile, it frequently saps a person of their overall wellness. In fact, back pain at present ranks third as a cause of poor health amid Americans, following middle affliction and chronic obstructive pulmonary disease (COPD).
In other words, getting people with spinal conditions back to work faster and with fewer complications has economic and social benefits likewise as health advantages.
Making Surgery Accessible to More People
By assuasive patients to avoid general anesthesia, Mummaneni's new approach makes dorsum surgery accessible to a broader range of people. That grouping includes most patients who would benefit from traditional spinal fusion or decompression surgery, besides as many who have difficulty tolerating general anesthesia, such as elderly patients.
In addition, the awake surgery appeals to those who are deterred from the traditional operation past the recovery time of a week or more.
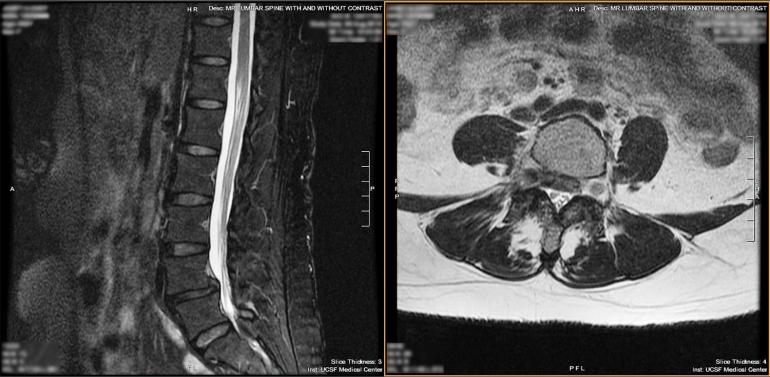
To determine whether a patient is a adept candidate for awake surgery, Mummaneni reviews the MRI and clinic notes. Awake surgery is currently bachelor for one- or ii-level lumbar procedures for decompression and/or fusion to treat stenosis and spondylolisthesis. UCSF is one of the get-go major medical centers in the U.Due south. to offering awake spine surgery through an Enhanced Recovery Subsequently Surgery (ERAS) protocol.
David had seen his share of dorsum issues when he contacted Mummaneni concluding summer. "I've had so many surgeries," he said. "I'g hardly a rookie with this."
Despite previous spinal procedures done at other hospitals, David experienced persistent back hurting, and he'd been referred to Mummaneni past some other surgeon. When the UCSF doctor offered him the opportunity for spine surgery without general anesthesia, David opted for it.
"I have nada pain now," he said. "Information technology was less time in the infirmary, less touch on on your body, recovery is accelerated, and there'southward less need to utilize hurting meds."
Source: https://www.ucsf.edu/news/2019/03/413446/spine-surgery-while-patients-are-awake-speeds-healing#:~:text=Benefits%20of%20Awake%20Spine%20Surgery&text=A%20traditional%20spinal%20fusion%20surgery,the%20hospital%20within%2024%20hours.
Posted by: andujarhoucter.blogspot.com

0 Response to "How Long Does Spinal Surgery Take"
Post a Comment